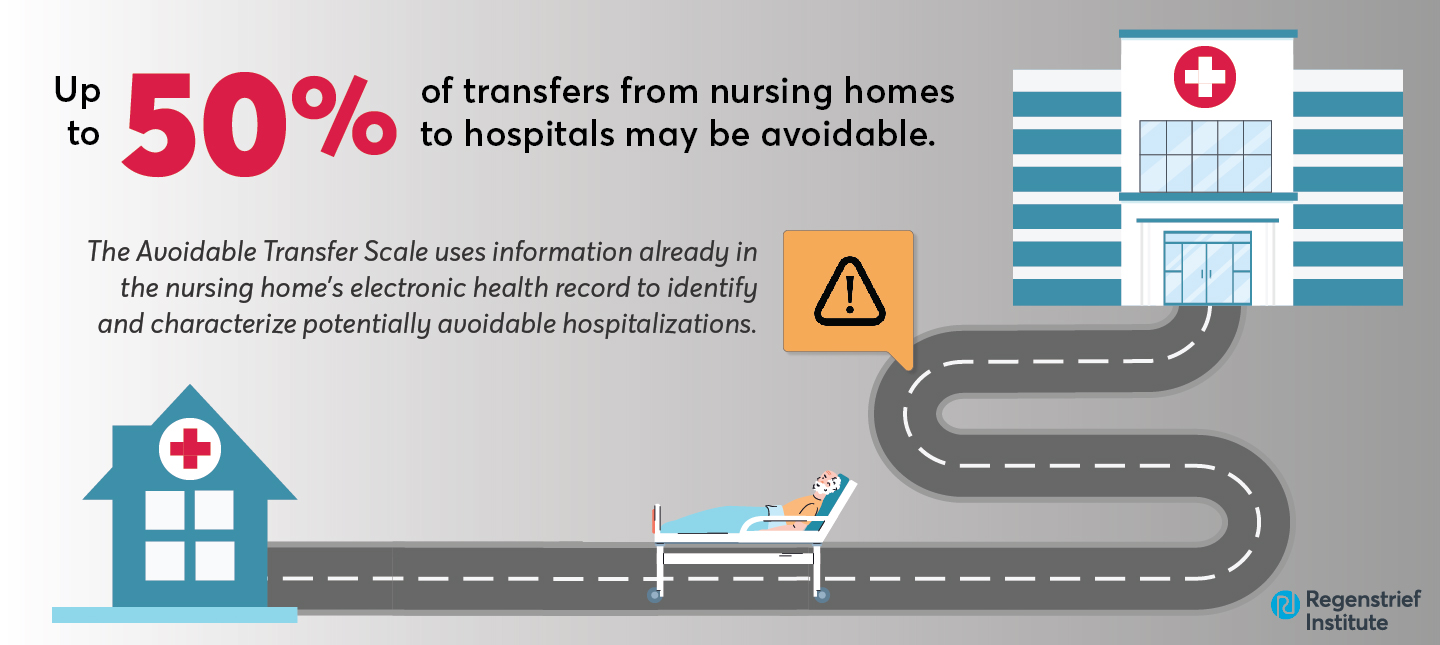
The Avoidable Transfer Scale, an innovative tool that uses data commonly included in a nursing home resident’s electronic medical record to identify and characterize potentially avoidable hospitalizations, highlights issues that can be handled in the nursing home itself.
The initial stage of the scale has been developed and pilot-tested by researcher-clinicians from the Regenstrief Institute and Indiana University School of Medicine with the dual ultimate use goals of helping nursing homes identify transfers to hospitals that can be avoided and to focus on trends in this arena that the facility may wish to address.
Although the definition of “avoidable” varies, it is estimated that between a quarter and as many as half of transfers of nursing home residents to hospitals are potentially avoidable. These transfers serve as both measures of quality in medical care and as important targets for process change by nursing homes.
Reducing the incidence of potentially avoidable hospital transfers benefits nursing home residents, many of whom are frail and/or cognitively impaired older adults for whom transfers are likely expensive, difficult and disruptive for patients as well as their families. Additionally, these transfers can be costly to the healthcare system in terms of unnecessary procedures and expenditures.
Importantly, the new tool enables nursing homes to outsource quality improvement work related to potentially avoidable hospitalizations. This may be critical during emergency situations like the COVID-19 pandemic or other infection outbreaks as well as other times when facilities are faced with lack of onsite staff available to focus on quality improvement.
“In nursing homes, the majority of potentially avoidable hospitalizations are linked to one of five medical conditions: pneumonia, heart failure, urinary tract infection, dehydration and asthma, but we need to get away from just using diagnoses to classify a transfer as avoidable. The Avoidable Transfer Scale clearly illustrates what the nursing home staff did to determine whether a transfer was needed or not,” said Geriatrician and study corresponding author Jennifer Carnahan, M.D., MPH, M.A., of the Regenstrief Institute and IU School of Medicine. “The transfer might not be avoidable if the nursing home has gone through all the processes to avoid it and the transfer moved forward. Or a transfer of a resident with one of these diagnoses or a different diagnosis might have been avoidable if certain prompts from our new tool had been addressed.”
Among the scale’s prompts:
- A pertinent nursing assessment was completed (within 12 hours) prior to transfer
- Warning signs of change in condition were reported by staff to a supervisor
- Goals of care were honored at the time of transfer
- Available diagnostic services were utilized to evaluate/diagnose the change in condition
- At the time of transfer, the resident’s condition could not be safely assessed in the facility
Prevention of avoidable transfers of nursing home patients has been a major focus of the IU Center for Aging Research at Regenstrief Institute since the $30.3 million Centers for Medicare and Medicaid (CMS) 2012-2020 funded OPTIMISTIC project — Optimizing Patient Transfers, Impacting Medical quality and Improving Symptoms: Transforming Institutional Care.
“The Avoidable Transfer Scale: A New Tool for Identifying Potentially Avoidable Hospital Transfers of Nursing Home Residents” appears in Innovation in Aging, an official journal of the Gerontological Society of America.
Authors of the study in addition to Dr. Carnahan are Kathleen T. Unroe, MHA, M.D. and Alexia M. Torke, M.S., M.D., Regenstrief Institute and IU School of Medicine; Russell Evans, MHA and Sarah Klepfer, R.N., Probari, Inc.; and Timothy E. Stump, M.A., and Patrick O. Monahan, PhD, both of IU School of Medicine.
The study was supported by the National Institutes of Health’s National Institute on Aging awards to Dr. Carnahan and Dr. Torke.
About Jennifer Carnahan, M.D., MPH, M.A.
In addition to her role as a research scientist at Regenstrief Institute, Jennifer Carnahan, M.D., MPH, M.A., is an assistant professor of medicine at Indiana University School of Medicine.
About Regenstrief Institute
Founded in 1969 in Indianapolis, Regenstrief Institute is a local, national and global leader dedicated to a world where better information empowers people to end disease and realize true health. A key research partner to Indiana University, Regenstrief and its research scientists are responsible for a growing number of major healthcare innovations and studies. Examples range from the development of global health information technology standards that enable the use and interoperability of electronic health records to improving patient-physician communications, to creating models of care that inform practice and improve the lives of patients around the globe.
Sam Regenstrief, a nationally successful entrepreneur from Connersville, Indiana, founded the institute with the goal of making healthcare more efficient and accessible for everyone. His vision continues to guide the institute’s research mission.
About IU School of Medicine
IU School of Medicine is the largest medical school in the U.S. and is annually ranked among the top medical schools in the nation by U.S. News & World Report. The school offers high-quality medical education, access to leading medical research and rich campus life in nine Indiana cities, including rural and urban locations consistently recognized for livability.