Study shows need for enhanced supportive oncology care
During active cancer treatment, patients express different needs than their caregivers, but both should be addressed to enhance the quality and value of supportive oncology care delivery. A new paper from Regenstrief Institute, Indiana University School of Nursing and University of Pennsylvania analyzed priorities of patients undergoing curative treatment and their caregivers to give a better understanding of how to support both.
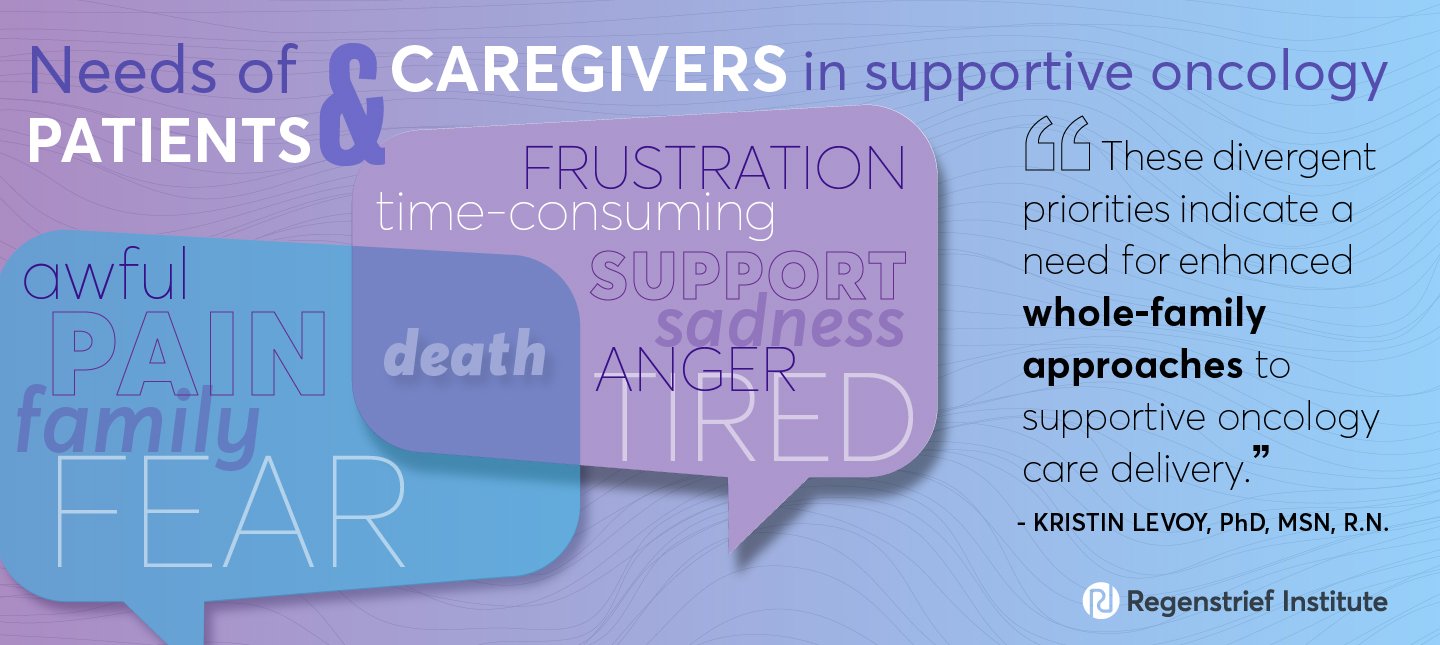
“In this study, we sought to identify which of the five supportive oncology domains — informational, physical, emotional, social and spiritual — were of greatest concern to patients and caregivers during active cancer treatment. We found that while both patients and caregivers cognitively prioritized concerns under the emotional domain, patients otherwise prioritized physical issues such as pain, and caregivers prioritized social issues such as supportive resources to help manage the patients’ care,” said first author Kristin Levoy, PhD, MSN, R.N., research scientist at IU Center for Aging Research at Regenstrief Institute and assistant professor at IU School of Nursing. “These divergent priorities indicate a need for enhanced whole-family approaches to supportive oncology care delivery which more readily account for the unique needs of both patients and caregivers at the time of cancer treatments to enhance the quality of care earlier in the cancer care continuum,” added Dr. Levoy.
Researchers used Freelisting, a method commonly used in cognitive anthropology, that allowed participants to generate a Freelist of in-the-moment illness concerns, rather than choosing from a preset inventory.
Analysis found that patients’ primary concerns were:
1. Pain
2. Death
3. Fear
4. Family
5. Awful
Caregivers listed:
1. Sadness
2. Time-consuming
3. Support
4. Anger
5. Tired
6. Death
7. Frustration
A version of the integrated findings can be found as an addendum to this release.
“Of particular significance to our team was that the caregiver interviews revealed that their priority concerns were not exclusively rooted in the patients’ needs, but also stemmed from their own significant emotional and social needs,” mentioned Dr. Levoy.
Study authors concluded that more concerted efforts to assess and integrate both patients and caregivers at the point of care are needed during active cancer treatments. The researchers suggest that Freelisting methods at the point of care may serve as a time-efficient way for the oncology team to steer care delivery in the direction of the issues that are of most concern in the moment, that is, providing “the ‘right’ care at the ‘right’ time to those patients and caregivers most in need.”
“It’s Rougher on Me Than It Is on Him”: Family Caregiver–Generated and Prioritized Illness Concerns While Patients Undergo Cancer Treatments” is published in the JCO® Oncology Practice.
In addition to Dr. Levoy, other authors on this paper are Jesse Wool, MBE, R.N., of the University of Pennsylvania School of Nursing and the Children’s Hospital of Philadelphia; Rebecca L. Ashare, PhD, of University of Buffalo; William E. Rosa, PhD, MBE, of Memorial Sloan Kettering Cancer Center; Frances K. Barg, PhD, of Perelman School of Medicine; and Salimah H. Meghani, PhD, MBE, R.N., of the University of Pennsylvania School of Nursing.
This research was supported by the American Cancer Society Grant ACS #128779-PEP-15-186. Additional author support included funding from an NIA/NINR award (R01 NR017853), an NIH/NINR Ruth L. Kirschstein National Research Service Award program (T32 NR009356), Novo Nordisk, Inc., an NIH/NCI Cancer Center Support Grant (P30 CA008748), and an NCI award program (T32 CA009461).
About Kristin Levoy, PhD, MSN, R.N., OCN, CNE
In addition to her role as a research scientist in the IU Center for Aging Research at Regenstrief Institute, Dr. Levoy is an assistant professor at the IU School of Nursing and an associate member of the IU Melvin and Bren Simon Comprehensive Cancer Center.
About Regenstrief Institute
Founded in 1969 in Indianapolis, Regenstrief Institute is a local, national and global leader dedicated to a world where better information empowers people to end disease and realize true health. A key research partner to Indiana University, Regenstrief and its research scientists are responsible for a growing number of major healthcare innovations and studies. Examples range from the development of global health information technology standards that enable the use and interoperability of electronic health records to improving patient-physician communications, to creating models of care that inform practice and improve the lives of patients around the globe.
Sam Regenstrief, a nationally successful entrepreneur from Connersville, Indiana, founded the institute with the goal of making healthcare more efficient and accessible for everyone. His vision continues to guide the institute’s research mission.
About IU School of Nursing
Indiana University School of Nursing is one of the largest nursing schools in the nation that offers a full range of programs from undergraduate to doctoral. Over 22,000 IUSON alumni across the globe are empowered to be leaders in clinical practice, research, education, and innovation. The School’s DNP program is ranked #1 in Indiana according to 2022 U.S. News & World Report Best Graduate Schools Rankings with the master’s program ranked in the top 50 in the United States.
Addendum*
Supportive Oncology Domain |
PatientFreelist Item (Rank) |
CaregiverFreelist Item (Rank) |
Qualitative Quote |
|---|---|---|---|
| Informational | — | — | “I didn’t really care because I was so overwhelmed with what was really happening that this isn’t something that you can go to school and have preparation for and take a Diagnosis of Cancer 101 course […] but the average person that’s not something that they do so that was something that we were thrown into […] I didn’t really get good advice. It was more like I needed to know the question to ask before they could give me the answer instead of me…” |
| Physical | Pain (1st) | Tired (5th) | “My experience is the medication does not seem to work for her pain that she is going through. That is what I was—that was my thoughts, is just the medication is not working” |
| Emotional | Death (2nd)
Fear (3rd) Awful (5th) |
Sadness (1st)
Anger (4th) Death (6th) Frustration (7th) |
“His body never gets a chance to recuperate anymore. We never get a chance to have any breathing space. We get through one hurdle, and then another one occurs. […] Sometimes, I feel I look worse than he does. I feel that it’s rougher on me than it is on him. Maybe it’s the way I handle things versus the way he does. It can be challenging. For a while I was seeing someone. I was speaking with someone.” |
| Social | Family (4th) | Time (2nd)
Support (3rd) |
“To me, that seems like it should be, the whole expectation that families should take care of it [general patient care], is a little unsettling. […] You want to give everything that you can, but at the same time, you worry about yourself, too.” |
| Spiritual | — | — | — |
*Researchers used qualitative interviews to add explanatory insights and to map the Freelist items to their relevant supportive oncology domain.