New understanding of pain over time may alter care and improve quality of life
Despite awareness that pain is common in nursing home residents, there has been minimal attention focused on how this pain changes over time. A new study from Regenstrief Institute and Indiana University School of Nursing researchers presents compelling evidence of the existence of four distinct pain trajectories in this population.
This new understanding of pain over time can help nursing home staff and clinicians better understand, recognize and respond to risk factors associated with persistent pain in individuals living in nursing homes. Ultimately, consideration of pain trajectories may alter courses of care and illness, prevent adverse outcomes and improve quality of life.
“Identification of pain trajectories can help us improve pain control for nursing home residents,” said Connie Cole, PhD, DNP, APRN, corresponding and lead author of the study. “We can identify risk factors, such as obesity or fracture, and use those to recognize individuals who are at increased risk for pain. For patients who are not able to self-report, such as someone with Alzheimer’s disease, we can use those factors to identify that they might be at increased risk for pain and therefore monitor them more closely.”
Persistent pain is associated with increased likelihood of depression, sleep problems, decreased happiness and diminished life satisfaction resulting in reduced quality of life and poorer health outcomes.
“This work highlights that pain is undertreated among many populations, including older adults in nursing homes. It’s critical that we continue to shine a spotlight on the unmet needs of these vulnerable individuals,” said study senior author Susan Hickman, PhD, director of Indiana University Center for Aging Research at Regenstrief Institute and interim president and CEO of the Institute.
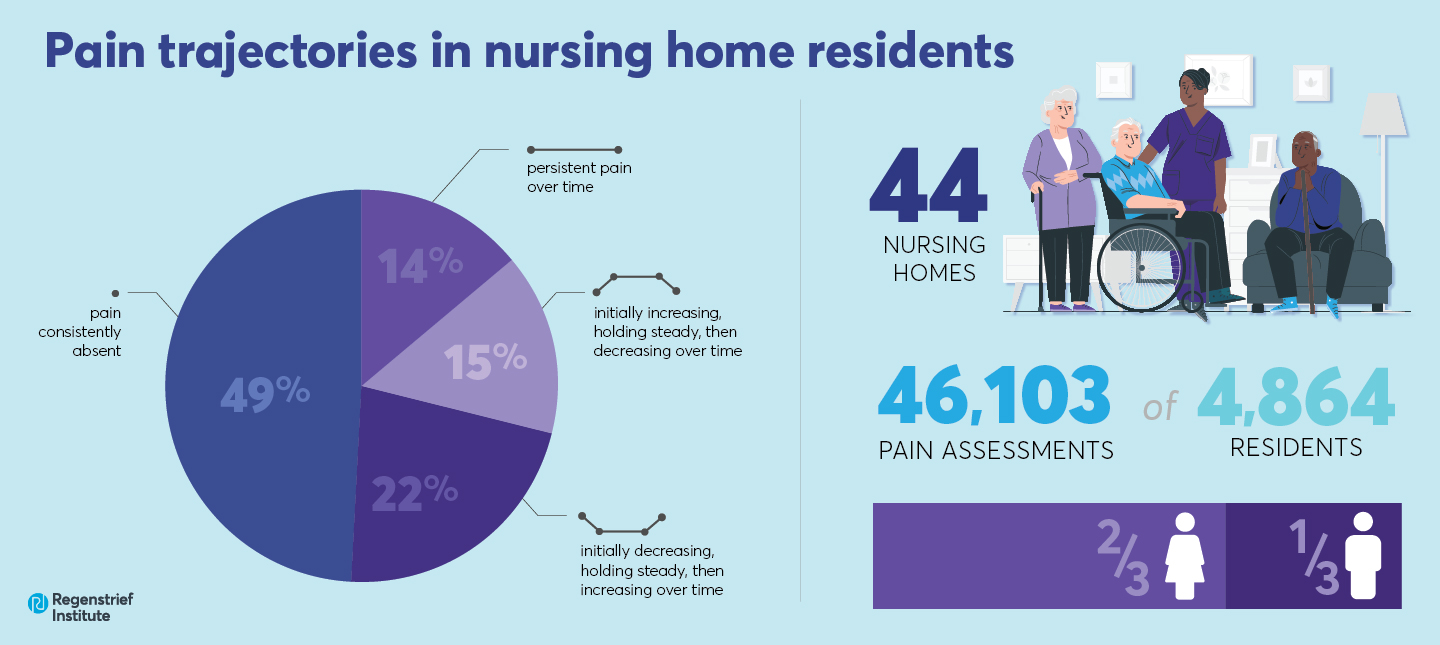
A total of 46,103 pain assessments of 4,864 nursing home residents, nearly two-thirds of whom were female, from 44 facilities were analyzed in the study.
The researchers identified four distinct long-term pain trajectories.
- persistent pain over time (14 percent)
- pain initially increasing, holding steady and then decreasing over time (15 percent)
- pain initially decreasing, holding steady and then increasing over time (22 percent)
- pain consistently absent (49 percent)
Among the study’s numerous findings regarding risk factors associated with various pain trajectories:
- Obesity and intact cognition were associated with the persistent pain presence trajectory as was living in a rurally located nursing home.
- Hip fracture was associated with a five-fold increased risk of persistent pain.
- Residents in the increasing-decreasing pain trajectory were at greater risk of death.
- Female gender, living in a rurally located nursing home, intact cognition and contracture (a condition of shortening and hardening of muscles) were common factors associated with all three of the trajectories in which pain was present.
- Nursing home residents with normal body mass index (BMI) or a diagnosis of Alzheimer’s disease or related dementia were less likely to be in any of the three trajectories in which pain was present.
“As a clinician, my experience has been that nursing home residents with a diagnosis of Alzheimer’s disease or dementia are less likely to be in any of the three trajectories with pain than those with intact cognition, due to inability to communicate and the difficulty in clinically evaluating pain in cognitively impaired individuals,” said Dr. Cole, who has worked as a nurse practitioner. “Identifying residents likely to be underrepresented in the pain trajectories may provide impetus for nursing home staff to improve pain assessment and evaluation.”
“The idea that there are trajectories of pain has relevance for a broader patient population beyond the nursing home setting,” added Dr. Hickman. “There is pressing need to better understand pain, how it changes over time, and what risk factors are associated, in particular, among older adults and those with cognitive impairment who are unable to express and report their own experiences.”
“Pain trajectories of nursing home residents” is published in the Journal of the American Geriatrics Society. Authors of the study, in addition to Drs. Cole and Hickman, are Janet S. Carpenter, PhD, R.N., IU School of Nursing; Justin Blackburn, PhD, IU Richard Fairbanks School of Public Health; Chen X. Chen, PhD, IU School of Nursing and Bobby L. Jones, PhD, University of Pittsburgh Medical Center.
This work was supported in part by a Luella McWhirter Fellowship, a Lyons Dissertation Award and a Woltman Communication in End-of-Life Fellowship.
About Susan Hickman, PhD
In addition to leading the IU Center for Aging Research at Regenstrief Institute, Dr. Susan Hickman is a professor at Indiana University School of Nursing, a professor and Cornelius and Yvonne Pettinga Chair of Aging Research at IU School of Medicine, and the co-director of the IUPUI Research in Palliative and End-of-Life Communicating and Training (RESPECT) Signature Center. Since June 2022 she has served as interim president and chief executive officer of the Regenstrief Institute.
About Connie Cole, PhD, DNP, APRN
Connie Cole earned a doctorate from Indiana University School of Nursing and is a postdoctoral palliative care and aging research fellow at the University of Colorado. She has extensive clinical experience with nursing home residents as a nursing assistant, director of nursing, nurse assessment coordinator and nurse practitioner.
About Regenstrief Institute
Founded in 1969 in Indianapolis, the Regenstrief Institute is a local, national and global leader dedicated to a world where better information empowers people to end disease and realize true health. A key research partner to Indiana University, Regenstrief and its research scientists are responsible for a growing number of major healthcare innovations and studies. Examples range from the development of global health information technology standards that enable the use and interoperability of electronic health records to improving patient-physician communications, to creating models of care that inform practice and improve the lives of patients around the globe.
Sam Regenstrief, a nationally successful entrepreneur from Connersville, Indiana, founded the institute with the goal of making healthcare more efficient and accessible for everyone. His vision continues to guide the institute’s research mission.
About IU School of Nursing
Indiana University School of Nursing was established in 1914 with the opening of Long Hospital in Indianapolis, Indiana. The School unites into a core structure with three campus locations: Bloomington, Indianapolis (IUPUI), and Fort Wayne. Almost 23,000 alumni across the globe are leaders in clinical practice, research, education, and innovation. The Master’s and DNP programs were named to the 2023 U.S. News & World Report Best Graduate Nursing Schools and in 2023 U.S. News & World Report Best Online Programs ranked the Master’s #10 in the nation. The National League for Nursing has designated the School as a Center of Excellence in Nursing Education in two areas. Academic programs include three tracks in the undergraduate program, nine tracks in the master’s program, post-master’s options, a post-masters DNP, and a PhD. The School is known for a robust program of research focused on quality of life in chronic illness, nursing education, and cancer prevention and control.