Study underscores importance of targeted health funding for rural communities
A study from Regenstrief Institute and Indiana University Richard M. Fairbanks School of Public Health researchers is one of the first to provide insight into health and behaviors of reproductive-age women in the rural Midwest before and between pregnancies. This population is at risk for poor health and pregnancy outcomes but, typically, is underrepresented in national, statewide and other public health studies.
The study revealed both poor preconception and poor interconception health status among rural women. An estimated 18 million women of reproductive age live in rural areas of the U.S.
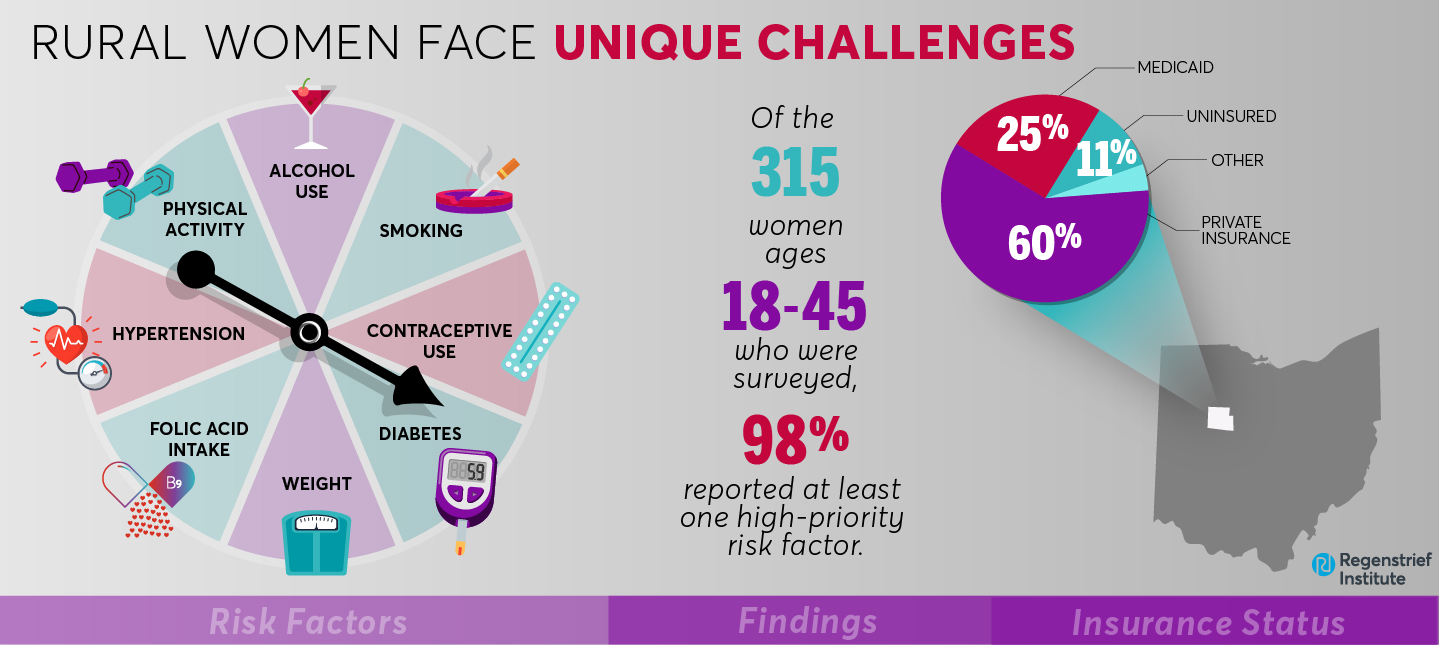
Approximately 98 percent of the 315 rural women surveyed by the researchers reported at least one high-priority risk factor related to smoking, hypertension, diabetes, alcohol use, folic acid intake, weight, physical activity or contraceptive use.
These women, who resided in northwest Ohio, fared worse than those in the state overall in smoking, folic acid intake, weight and hypertension, making the rural women more vulnerable to poor pregnancy outcomes and at higher risk for worse overall health outcomes such as diabetes, obesity and cancer.
Although the survey responses suggested that most study participants did not meet the threshold for heavy alcohol use, nearly one-third reported recent episodes of binge drinking.
“Our findings highlight some of the disparities between rural women and other women in Ohio, which may reflect a bias toward the urban populations,” said Regenstrief and Fairbanks School researcher Brian Dixon, PhD, MPA, senior author of the study. “So that means that if we are thinking about how to reduce rates of cancer and how to address the health of these women and exposure of their children to secondhand smoke, we need to put more resources into smoking cessation programs at the rural level.”
The study was conducted in Hardin County, a rural county of 470 square miles with a total population of 31,480 and a shortage of healthcare professionals. Kenton, the largest city in the county, has a population of fewer than 8,000.
Survey responses were collected from women at multiple locations across the county. Ages ranged from 18 to 45 and they were not pregnant. Approximately 96 percent were White, consistent with county demographics. Three quarters had one or more children. About 60 percent had private health insurance and nearly a quarter qualified for Medicaid. Approximately 11 percent had no health insurance.
”Statewide estimates are often used to track preconception and interconception health status for reproductive-age women; however, this may not portray the actual health status for women living in rural or underserved areas,” said Natalie DiPietro Mager, PharmD, PhD, first author of the study, who teaches at Ohio Northern University. “The findings of this study show that we need better methods to collect and report data for women in these areas so that needed interventions can be identified.”
The findings of this study can be used for monitoring, comparison, and benchmarking.
The authors note that the study “identified important health risks that should be prioritized and addressed through clinical and public health interventions that account for the unique challenges faced by rural women.” They observe that their “findings underscore the importance of targeted funding for rural communities to improve residents’ health and decrease health disparities.”
“Preconception health status and associated disparities among rural, Midwestern women in the United States” is published in the peer-reviewed journal Birth: Issues in Perinatal Care.
Study authors, as listed in the publication
Natalie A DiPietro Mager 1,6, Terrell W Zollinger 1, Jack E Turman Jr 2 3, Jianjun Zhang 1 4, Brian E Dixon 1 5
Affiliations, as listed in the publication
1Department of Epidemiology, Indiana University Richard M. Fairbanks School of Public Health, Indianapolis, Indiana, USA.
2Department of Social and Behavioral Sciences, Indiana University Richard M. Fairbanks School of Public Health, Indianapolis, Indiana, USA.
3Department of Pediatrics, Indiana University School of Medicine, Indianapolis, Indiana, USA.
4Indiana University Melvin and Bren Simon Comprehensive Cancer Center, Indianapolis, Indiana, USA.
5Center for Biomedical Informatics, Regenstrief Institute, Inc., Indianapolis, Indiana, USA.
6Ohio Northern University, Raabe College of Pharmacy, Ada, Ohio, USA.
About Brian E. Dixon, PhD, MPA
In addition to his roles as interim director of the Regenstrief Institute’s Clem McDonald Center for Biomedical Informatics and director of public health informatics for Regenstrief Institute and Indiana University Richard M. Fairbanks School of Public Health, Brian E. Dixon, PhD, MPA, is a professor of epidemiology at the Fairbanks School of Public Health. He is also an affiliate scientist at the U.S. Department of Veterans Affairs Health Services Research and Development Center for Health Information and Communication, Richard L. Roudebush VA Medical Center.
About Regenstrief Institute
Founded in 1969 in Indianapolis, the Regenstrief Institute is a local, national and global leader dedicated to a world where better information empowers people to end disease and realize true health. A key research partner to Indiana University, Regenstrief and its research scientists are responsible for a growing number of major healthcare innovations and studies. Examples range from the development of global health information technology standards that enable the use and interoperability of electronic health records to improving patient-physician communications, to creating models of care that inform practice and improve the lives of patients around the globe.
Sam Regenstrief, a nationally successful entrepreneur from Connersville, Indiana, founded the institute with the goal of making healthcare more efficient and accessible for everyone. His vision continues to guide the institute’s research mission.
About the IU Richard M. Fairbanks School of Public Health
Located on the IUPUI and Fort Wayne campuses, the IU Richard M. Fairbanks School of Public Health is committed to advancing the public’s health and well-being through education, innovation and leadership. The Fairbanks School of Public Health is known for its expertise in biostatistics, epidemiology, cancer research, community health, environmental public health, global health, health policy and health services administration.