Underlying causes still unknown, including patient, family or group preferences
INDIANAPOLIS – In one of the first studies to investigate racial disparities in the pharmacologic treatment of insomnia, researchers from Regenstrief Institute and Indiana University report that patients belonging to racial minority groups were significantly less likely to be prescribed medication following diagnosis of insomnia than White patients.
The study found that Black patients were much less likely to have been prescribed an FDA-approved insomnia medication at any time post diagnosis than White patients. Other non-White individuals were significantly less likely to be prescribed an FDA-approved medication two, three, and four years after insomnia diagnosis but not in year one.
“We looked at comorbidities — anxiety disorders and depression — and we looked at where individuals lived and other factors that might account for the disparity in prescriptions for medications following a diagnosis of insomnia,” noted co-author and Regenstrief Research Scientist Malaz Boustani, M.D., MPH. “We found that race was the only variable that accounted for the differences in treatment.”
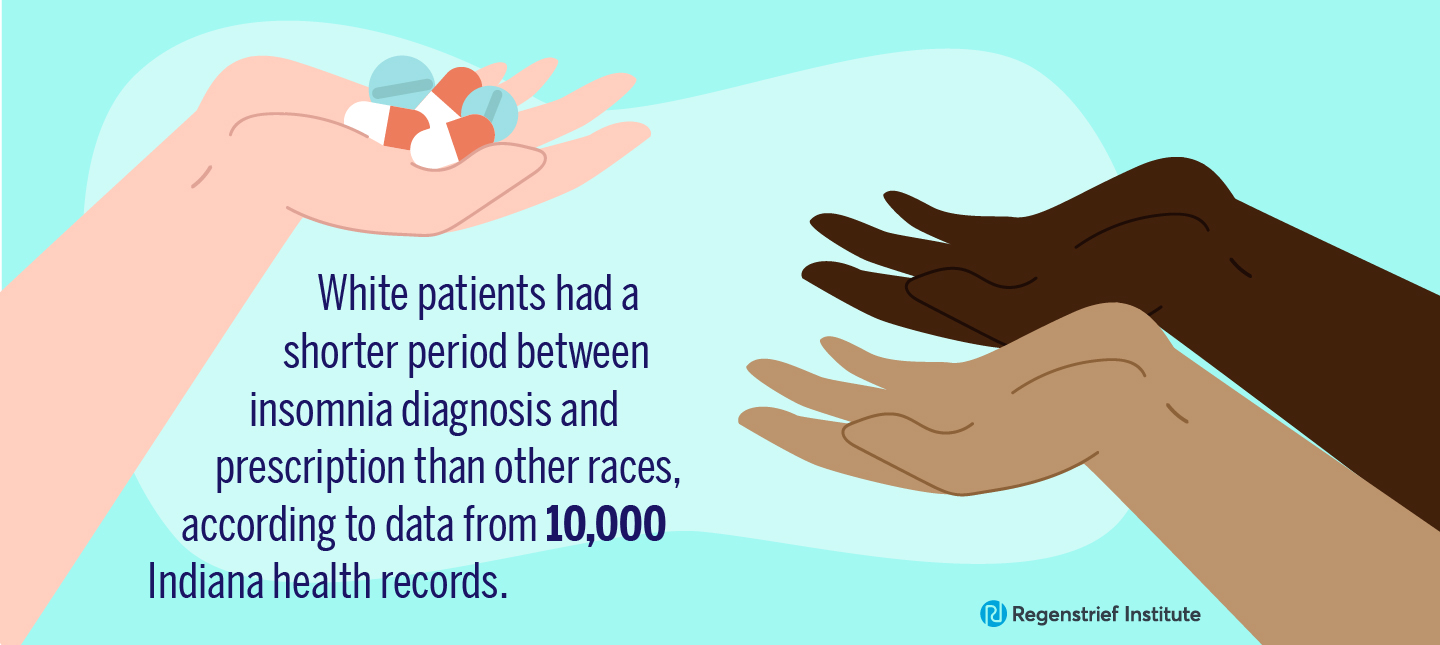
The researchers reported that despite older patients and those with comorbidities being less likely to be prescribed insomnia medications regardless of race, White patients overall still had a shorter period between diagnosis and prescription than other races.
Insomnia is a common sleep disorder involving difficulty falling asleep, staying asleep or getting good-quality sleep. According to the U.S. Centers for Disease Control and Prevention, not getting enough sleep is linked with many chronic diseases and conditions including type 2 diabetes, heart disease, obesity and depression.
“We did this study to simply identify treatment trends,” said Regenstrief Institute Research Scientist Noll Campbell, PharmD, M.S., a study co-author. “Are the trends we found caused by individual patient preferences, group-based preferences, or are they the result of different approaches to nonpharmacologic options for the treatment of insomnia? Future research will be needed to discern why these trends are occurring.”
In this study, data from the Indiana Network for Patient Care (INPC) included about 10,000 individuals who were prescribed FDA-approved medications for insomnia was analyzed. The INPC is managed by the Indiana Health Information Exchange. Regenstrief created the INPC and provides access to data for research purposes.
“The Indiana Network for Patient Care proved once again to be an invaluable resource for understanding clinical practice. It was only through the INPC that we obtained the demographic, diagnostic, medication, and clinical notes data necessary for analyzing racial disparities in insomnia medication prescribing,” said Regenstrief Institute Research Scientist Paul Dexter, M.D., a study co-author and clinician-informatician.
“The systematic analysis of electronic health records data can play an important role in helping us uncover disparities that can be acted upon towards more equitable care,” said Regenstrief Institute Research Scientist Arthur Owora, PhD, MPH, the study senior author. “This potential is highlighted by this study; however, given the inherent deficits of secondary data sources, a cautious interpretation is warranted, and further research is needed to better understand how and to what extent patient preferences and patient-clinician interactions may have contributed to the observed disparities in insomnia treatment.”
The study population was 75 percent White, 69 percent female and 62 percent non-Hispanic. Average age at the time of insomnia diagnosis was 61.
“In addition to revealing racial disparity in prescription of medications for insomnia, the data suggests that providers may be undertreating insomnia,” said study first author Emma Holler, MPH, a doctoral student and clinical epidemiologist with Indiana University School of Public Health — Bloomington.
“Racial disparities in the pharmacological treatment of insomnia: A time-to-event analysis using real-world data” is published in the peer-reviewed journal Sleep Medicine.
This work was supported in part by Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc.
Authors
Emma Holler 1, Noll L. Campbell 2, Malaz Boustani 3, Paul Dexter 4, Zina Ben Miled 5, Arthur Owora 6.
Affiliations
1 Department of Epidemiology and Biostatistics, Indiana University Bloomington, Bloomington, Indiana, USA. Electronic address: emorone@iu.edu.
2 College of Pharmacy, Purdue University, West Lafayette, Indiana, USA; Indiana University Center for Aging Research, Regenstrief Institute, Indianapolis, Indiana, USA; Center for Healthcare Innovation and Implementation Science, Indiana University, Indianapolis, Indiana, USA.
3 Indiana University Center for Aging Research, Regenstrief Institute, Indianapolis, Indiana, USA; Center for Healthcare Innovation and Implementation Science, Indiana University, Indianapolis, Indiana, USA; Department of Internal Medicine, Indiana University School of Medicine, Indianapolis, Indiana, USA.
4 Department of Internal Medicine, Indiana University School of Medicine, Indianapolis, Indiana, USA; Clem McDonald Center for Biomedical Informatics, Regenstrief Institute, Indianapolis, Indiana, USA.
5 Department of Electrical and Computer Engineering, Indiana University Purdue University at Indianapolis, Indianapolis, Indiana, USA.
6 Department of Epidemiology and Biostatistics, Indiana University Bloomington, Bloomington, Indiana, USA.
About Malaz Boustani, M.D., MPH
In addition to his role as a research scientist at Regenstrief Institute, Malaz Boustani, M.D., MPH, is the founding director of the Center for Health Innovation and Implementation Science. He is a professor and the Richard M. Fairbanks Professor in Aging Research at Indiana University School of Medicine. Dr. Boustani is also director of care innovation at Eskenazi Health.
About Noll Campbell, PharmD, M.S.
In addition to his role as a research scientist at Regenstrief Institute, Noll Campbell, PharmD, M.S., is an associate professor of pharmacy practice at the Purdue University College of Pharmacy. He is an adjunct associate professor of medicine at Indiana University School of Medicine and maintains an active clinical practice as a geriatric pharmacotherapy expert within Eskenazi Health.
About Paul R. Dexter, M.D.
In addition to his role as a research scientist at Regenstrief Institute, Paul R. Dexter, M.D., is an associate professor of clinical medicine at Indiana University School of Medicine.
About Arthur H. Owora, MPH, PhD
In addition to his role as a research scientist at Regenstrief Institute, Arthur H. Owora, PhD., is an associate professor of pediatrics at Indiana University School of Medicine. He is an adjunct associate professor of biostatistics and epidemiology at Indiana University School of Public Health-Bloomington.
About Regenstrief Institute
Founded in 1969 in Indianapolis, Regenstrief Institute is a local, national and global leader dedicated to a world where better information empowers people to end disease and realize true health. A key research partner to Indiana University, Regenstrief and its research scientists are responsible for a growing number of major healthcare innovations and studies. Examples range from the development of global health information technology standards that enable the use and interoperability of electronic health records to improving patient-physician communications, to creating models of care that inform practice and improve the lives of patients around the globe.
Sam Regenstrief, a nationally successful entrepreneur from Connersville, Indiana, founded the institute with the goal of making healthcare more efficient and accessible for everyone. His vision continues to guide the institute’s research mission.
About IU School of Medicine
IU School of Medicine is the largest medical school in the U.S. and is annually ranked among the top medical schools in the nation by U.S. News & World Report. The school offers high-quality medical education, access to leading medical research and rich campus life in nine Indiana cities, including rural and urban locations consistently recognized for livability.
About Purdue University College of Pharmacy
The mission of the Purdue University College of Pharmacy is to advance scientific discovery and development, maximize global health outcomes through patient care and public service, and educate and train students to become leading pharmacists and scientists. The goal is to transform the practice and science of pharmacy to lead advances in human health.
About IU School of Public Health-Bloomington
IU School of Public Health-Bloomington (SPH-B) is one of the largest schools of public health in the United States, offering top-ranked programs in a wide range of health-related fields. Accredited by the Council on Education for Public Health (CEPH), the school aims to promote health among individuals in Indiana, the nation, and the world through integrated multidisciplinary approaches to research and creative activities, teaching, and community engagement.