An interdisciplinary team from University of Wisconsin School of Medicine and Public Health, Regenstrief Institute and Indiana University School of Medicine will evaluate the effectiveness of the collaborative care model to prevent the development of Alzheimer’s disease and other related dementias among delirium survivors after emergency surgery using a randomized controlled trial.
The work is supported by a five-year grant expected to total more than $10 million from the National Institutes of Health’s National Institute on Aging.
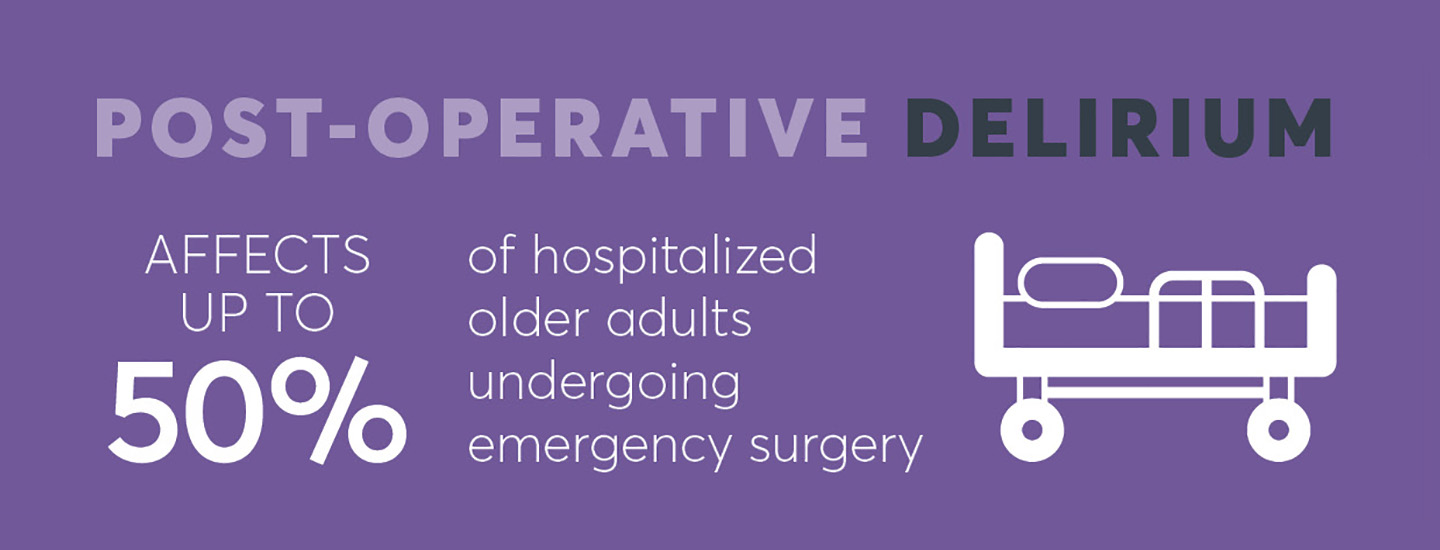
Post-operative delirium can lead to Alzheimer’s disease and other related dementias with resulting lower quality of life, loss of functional independence and high healthcare utilization. In 2020, the estimated societal cost of Alzheimer’s and related dementias was more than $300 billion and the projected annual economic cost for these conditions will exceed $1.5 trillion by 2050. Delirium — characterized by an acute change in attention, awareness or consciousness — affects up to 50 percent of hospitalized older adults undergoing emergency surgery and costs the healthcare system billions of dollars each year.
It is common for patients to experience grogginess and some confusion coming out of anesthesia, but post-operative delirium is far different and much more serious. It is not uncommon for post-operative delirium to lead to Alzheimer’s disease and other related dementias.
“Longer life expectancy places more older Americans at risk for Alzheimer’s disease and dementia diagnoses,” said Ben Zarzaur, M.D., MPH, a surgeon who specializes in trauma, emergency surgery and surgical critical care. He is faculty at UW School of Medicine and Public Health. “Wide implementation of collaborative care model interventions such as the EGS Delirium Recovery Model could lead to recovered cognitive function, significantly improved overall quality of life for a broad population of patients and their families, and a reduced cost burden to families and healthcare systems.”
“Surgical patients who suffer one episode of delirium have 12 times the likelihood of developing an Alzheimer’s or related dementia diagnoses within a year compared to similar surgical patients who do not experience delirium,” said Malaz Boustani, M.D., MPH, a geriatrician, a Regenstrief research scientist and faculty for IU School of Medicine. “We want to use our collaborative care model – Emergency General Surgery Delirium Recovery Model – to intervene and prevent ADRD among delirium survivors.”
Both Dr. Zarzaur and Dr. Boustani have personal connections that make this study especially important to them. Dr. Zarzaur’s mother and both of his grandmothers died as a result of Alzheimer’s disease-related disorders as did Dr. Boustani’s father.
Drawing upon lessons learned from chronic disease care, working directly with patients and their primary care and specialty providers, the dynamic, scalable new care model is a feedback loop designed to influence the patient’s recovery trajectory.
“Emergency General Surgery Delirium Recovery Model: A Collaborative Care Interview,” is supported by National Institutes of Health’s National Institute on Aging, grant R01AG076489. Study participants will be seen in hospitals in Indianapolis, Madison, Wisconsin and Rockford, Illinois.
In addition to Drs. Boustani and Zarzaur, other research collaborators include Babar Khan, M.D., M.S., Regenstrief and IU School of Medicine; Andrea Gilmore-Bykoyskyi, PhD, R.N., and Angela Ingraham, M.D., M.S., both of University of Wisconsin School of Medicine and Public Health; Fredrick Unverzagt, PhD, and Sujuan Gao, PhD, both of IU School of Medicine.
Malaz Boustani, M.D., MPH
In addition to his role as a research scientist with the Indiana University Center for Aging Research at Regenstrief Institute, Malaz Boustani, M.D., MPH, is the founding director of the Center for Health Innovation an Implementation Science. He is a professor and the Richard M. Fairbanks Chair in Aging Research at Indiana University School of Medicine. Dr. Boustani is also director of care innovation at Eskenazi Health.
Ben L. Zarzaur, M.D., MPH
In addition to being a general surgeon, Dr. Zarzaur is a member of the faculty of the University of Wisconsin School of Medicine and Public Health, where he is the Sylvia and Royal Lichtfeldt Professor and Division Chair of Acute Care and Regional General Surgery.
About Regenstrief Institute
Founded in 1969 in Indianapolis, the Regenstrief Institute is a local, national and global leader dedicated to a world where better information empowers people to end disease and realize true health. A key research partner to Indiana University, Regenstrief and its research scientists are responsible for a growing number of major healthcare innovations and studies. Examples range from the development of global health information technology standards that enable the use and interoperability of electronic health records to improving patient-physician communications, to creating models of care that inform practice and improve the lives of patients around the globe.
Sam Regenstrief, a nationally successful entrepreneur from Connersville, Indiana, founded the institute with the goal of making healthcare more efficient and accessible for everyone. His vision continues to guide the institute’s research mission.
About University of Wisconsin School of Medicine and Public Health
Founded in 1925 and recognized as an international leader in education, research and service, the University of Wisconsin School of Medicine and Public Health continues to evolve to meet changing healthcare needs. From treating individual patients to improving the health of populations, the UW School of Medicine and Public Health’s reach is visible through education, research, patient care and community service into all corners of the state. Service is engrained in the school’s mission, and it drives faculty, students and staff to move healthcare forward.
About IU School of Medicine
IU School of Medicine is the largest medical school in the U.S. and is annually ranked among the top medical schools in the nation by U.S. News & World Report. The school offers high-quality medical education, access to leading medical research and rich campus life in nine Indiana cities, including rural and urban locations consistently recognized for livability.