INDIANAPOLIS – Clinical trials are constantly being designed and study participants enrolled to determine if medical treatments and therapies are safe and effective. Much has been written about the importance of including diverse populations in these trials.
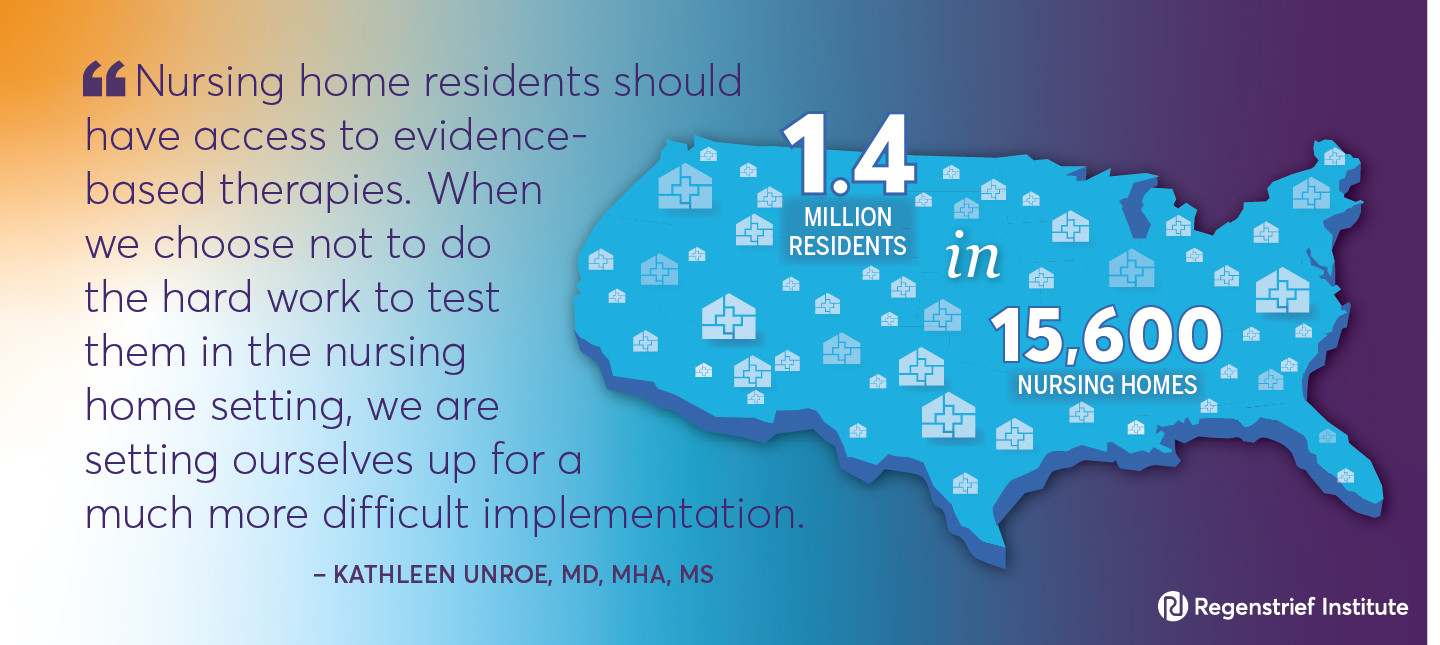
However, the nearly 1.4 million individuals who live in the 15,600 nursing homes across the U.S. have been largely left out of clinical trials, despite the prevalence of such common conditions as hypertension, depression, diabetes and Alzheimer’s disease in this population.
A commentary by faculty of Regenstrief Institute, Indiana University, UCLA and the universities of North Carolina, Colorado and Massachusetts, published in the Journal of the American Geriatrics Society (JAGS), focuses on the importance of including nursing home residents, a population with significant medical complexity, in clinical trials. The essay highlights the benefits and challenges of conducting research on medical therapies in nursing homes. The authors identify key elements for successful nursing home clinical trials and propose a nursing home clinical trials network, noting that ensuring diversity, equity and inclusion in any trial design is imperative.
“Among the questions we want to ask are: Is this therapy appropriate for a nursing home population? Does it work in a nursing home population but are there issues around implementation? Are there challenges to delivering it in a nursing home setting?” notes corresponding author Kathleen Unroe, M.D., MHA, M.S., a Regenstrief Institute and IU School of Medicine researcher-clinician. “Nursing homes were not built to facilitate research. We as researchers need to fit in. We need to appreciate the realities of providing clinical care in this setting and adjust and adapt our protocols to work within that system.”
Among the topics discussed in the commentary:
- The need for clinical trials in nursing homes
- Gaps that can be filled with these clinical trials
- Challenges conducting these clinical trials
- Next steps in conducting clinical trials in nursing homes
- A framework for making a nursing home clinical trials network a reality
“It is imperative that we build the science of nursing home care around testing, prevention, diagnosis, and treatment. It is a unique setting that merits more focus given the essential role it plays in the continuum of care for seriously ill adults,” said commentary co-author Susan Hickman, PhD, director of Regenstrief Institute’s Center for Aging Research and a faculty member of IU schools of nursing and medicine.
Citing a missed opportunity, the authors write, “Inclusion of nursing home residents in COVID-19 therapeutics trials might have identified specific issues relating to dosing, administration and monitoring, spurred creation of training materials specifically for nursing home staff, and promoted the development of consistent policies to identify appropriate candidates and deliver treatments promptly, safely, and optimally.”
Dr. Unroe adds, “Nursing home residents should have access to evidence-based therapies. When we choose not to do the hard work to test them in the nursing home setting, we are setting ourselves up for a much more difficult implementation.” She notes that “Conducting trials in the nursing home may generate generalizable knowledge that also would be highly relevant to people who are cared for in assisted living facilities or even the broader geriatric population living at home.”
“Evaluation of medical therapies in the nursing home population: Gaps, challenges, and next steps” is part of a JAGS special collection, “A changing landscape for evaluation of new therapies for older adults and diverse populations: National and international perspectives.”
Authors and affiliations:
Kathleen T. Unroe MD, MHA, MS1,2,3| Debra Saliba MD, MPH, AGSF4,5,6,7|Susan E. Hickman PhD2,3,8| Sheryl Zimmerman PhD9,10,11|Cari Levy MD, PhD12,13| Jerry Gurwitz MD14
1Division of General Internal Medicine and Geriatrics, Indiana University School of Medicine, Indianapolis, Indiana, USA
2Indiana University Center for Aging Research, Regenstrief Institute Inc., Indianapolis, Indiana, USA
3Research in Palliative and End-of-Life Communication and Training (RESPECT) Center, Indiana University School of Medicine, Indianapolis, Indiana, USA
4US Department of Veterans Affairs Greater Los Angeles Healthcare System (VAGLAS) Health Services Research and Development Service (HSR&D) Center of Innovation, Los Angeles, California, USA
5David Geffen School of Medicine, University of California, Los Angeles, California, USA
6Anna and Harry Borun Center for Gerontological Research, University of California Division of Geriatrics, Los Angeles, California, USA
7RAND Corporation, Santa Monica, California, USA
8Indiana University School of Nursing, Indianapolis, Indiana, USA
9School of Social Work, University of North Carolina, Chapel Hill, North Carolina, USA
10Cecil G. Sheps Center for Health Services Research, University of North Carolina, Chapel Hill, North Carolina, USA
11Center for Excellence in Assisted Living (CEAL), School of Social Work, University of North Carolina, Chapel Hill, North Carolina, USA
12Division of Geriatric Medicine, University of Colorado School of Medicine Anschutz Campus, Aurora, Colorado, USA
13Denver Veterans Affairs Medical Center, Aurora, Colorado, USA
14Division of Geriatric Medicine, UMass Chan Medical School, Worcester, Massachusetts, USA
Kathleen T. Unroe, M.D., MHA, M.S.
In addition to being a research scientist with the Indiana University Center for Aging Research at Regenstrief Institute, Kathleen Unroe, M.D., MHA, M.S., is an associate professor of medicine at Indiana University School of Medicine and a practicing geriatrician. Dr. Unroe is the founder and an executive officer of Probari, a healthcare start-up supporting nursing home care.
Susan Hickman, PhD
In addition to serving as director and a research scientist with the Indiana University Center for Aging Research at Regenstrief Institute, Susan Hickman, PhD, is a professor at Indiana University School of Nursing, a professor of medicine and the Cornelius and Yvonne Pettinga Professor of Aging Research at Indiana University School of Medicine and co-director of the IU Indianapolis Research in Palliative and End-of-Life Communicating and Training (RESPECT) Signature Center.