National expert panel issues strategy recommendations for policymakers and payers
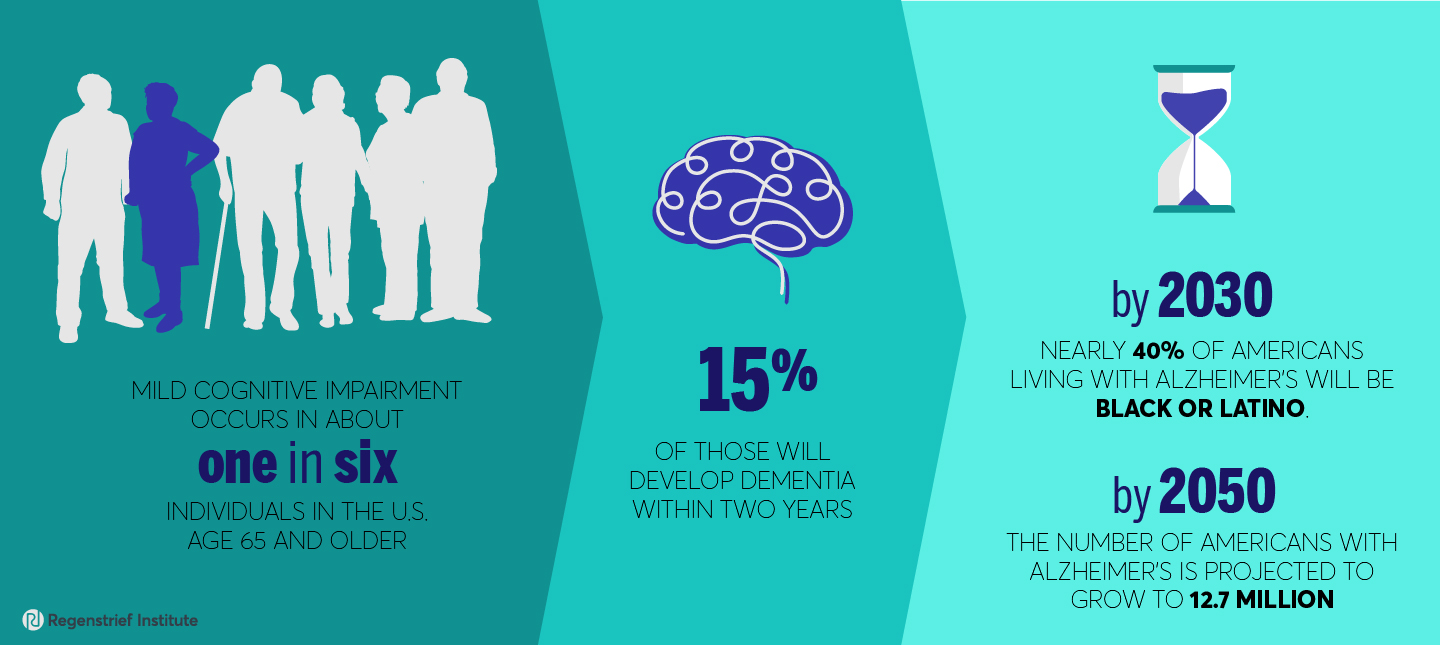
INDIANAPOLIS – Mild cognitive impairment, which occurs in about one in six individuals in the U.S., age 65 and older, remains substantially underdiagnosed, especially in disadvantaged populations.
Convened by the non-profit UsAgainstAlzheimer’s, The Brief Cognitive Assessment Work Group, is composed of 15 clinicians, researchers and health systems administrators from across the U.S. The group advocates for early detection of cognitive impairment to benefit both patients and caregivers by providing time to plan for future care, allowing preventive steps to potentially delay some symptoms as well as recognizing cognitive impairment due to a currently treatable condition.
The expert panel’s recommendations for policymakers and payers on strategies to promote widespread and equitable use of brief cognitive assessment tools in primary care is published in Alzheimer’s & Dementia, a peer-reviewed journal of the Alzheimer’s Association.
“Over the past 15 years, we and other researchers have been studying the risks and benefits of early detection of cognitive impairment and shown it can be beneficial and causes no harm, as measured by patient distress,” said work group member Nicole Fowler, PhD, MHSA, who is also a Regenstrief Institute research scientist and an Indiana University School of Medicine faculty member. “There have been policy changes to spur and increase detection in primary care, such as including screening for cognitive impairment in the Medicare Annual Wellness visit, but there has been little specificity – directions on how to accomplish this — given to providers.”
The routine use of brief cognitive assessment tools, which are not diagnostic, is a promising approach to improving cognitive impairment detection according to the work group. These tools are intended to help identify patients in need of full cognitive examination. The expert panel notes that brief cognitive assessments can address barriers that more in-depth cognitive assessments encounter, such as the limited time available during medical appointments and insufficient clinician training.
“The role of this paper was to be as specific as possible about what we actually need as a system to do this,” said Dr. Fowler. “For example, what kind of tools already exist to conduct cognitive impairment detection in primary care that are facile to use, that are easily integrated into the workflow? How can clinicians and healthcare systems potentially get reimbursed for screening for mild cognitive impairment?”
To address these and other challenges, the expert panel recommends:
- incorporating brief cognitive assessments into the regular workflow of primary care practices through the use of support team members.
- calling on professional societies, healthcare systems and other stakeholders to develop and broadly disseminate guidance on clinician communication of cognitive discussions with patients; and
- health systems configure electronic health records to incorporate brief cognitive assessments.
An estimated 15 percent of individuals with mild cognitive impairment will develop dementia within two years. By 2030 nearly 40 percent of Americans living with Alzheimer’s will be Black or Latino. By 2050 the number of Americans living with Alzheimer’s disease is projected to grow to 12.7 million.
“Expanding the use of brief cognitive assessments to detect suspected early-stage cognitive impairment in primary care” concludes, “…the long-standing neglect of detection of cognitive impairment has resulted in a hidden epidemic. As our under-standing of the biology of neurodegenerative diseases improves and better treatments emerge, concerted efforts from many stakeholders are necessary to identify patients who can benefit from those innovations, and do so in a timely and equitable manner.”
UsAgainstAlzheimer’s provided funding to facilitate the consensus-building process of the expert panel and support the drafting of the perspective paper.
Authors and affiliations
Soeren Mattke1,2, Donnie Batie1,3, Joshua Chodosh1,4,5, Kristen Felten1,6, Ellen Flaherty1,7,8, Nicole R. Fowler1,9,10,11, Fred A. Kobylarz1,12, Kelly O’Brien13, Russ Paulsen13, Anne Pohnert1,14, Katherine L. Possin1,15, Tatiana Sadak1,16, DianeTy1,17, Amy Walsh1,18, and Julie M. Zissimopoulos1,19.
1Brief Cognitive Assessment Work Group, District of Columbia, USA
2Center for Improving Chronic Illness Care, University of Southern California, Los Angeles, California, USA
3Baton Rouge General Medical Center, Baton Rouge, Louisiana, USA
4Division of Geriatric Medicine and Palliative Care, Department of Medicine, New York University School of Medicine, New York, New York, USA
5NYU School of Medicine, New York Harbor VA Healthcare System, New York, New York, USA
6Wisconsin Department of Health Services, Office on Aging, Madison, Wisconsin, USA
7Geisel School of Medicine, Dartmouth College, Lebanon, New Hampshire, USA
8Dartmouth Centers for Health and Aging, Geisel School of Medicine, Lebanon, New Hampshire, USA
9Indiana University Center for Aging Research, Indiana University School of Medicine and the Regenstrief Institute, Indianapolis, Indiana, USA
10Division of General Internal Medicine and Geriatrics, School of Medicine, Indianapolis, Indiana, USA
11Center for Health Innovation and Implementation Science, Indiana University, Indianapolis, Indiana, USA
12Department of Family Medicine and Community Health, Robert Wood Johnson Medical School, Rutgers Biomedical and Health Sciences, New Brunswick, New Jersey, USA
13Us Against Alzheimer’s, Washington, District of Columbia, USA
14CVS Health Minute Clinic, Woonsocket, Rhode Island, USA
15Department of Neurology, University of California, San Francisco Memory and Aging Center, San Francisco, California, USA USA
16University of Washington School of Nursing, Seattle, Washington, USA
17Alliance to Improve Dementia Care, Milken Institute Center For the Future of Aging, Washington, District of Columbia, USA
18Age-Friendly Health Systems, Institute for Healthcare Improvement, Boston, Massachusetts, USA
19Sol Price School of Public Policy, University of Southern California, Los Angeles, California, USA
In 2019, Dr. Fowler was corresponding author of a groundbreaking study which evaluated the pros and cons of population screening for dementia in primary care. The study found no harm, as measured by symptoms of depression or anxiety, from screening older adults for Alzheimer’s disease and related dementias. Co-authors include Regenstrief research scientists Greg A. Sachs, M.D., and Malaz Boustani, M.D., MPH.
About Nicole Fowler, PhD, MHSA
In addition to her role as a Regenstrief Institute research scientist and associate director of the IU Center for Aging Research at Regenstrief Institute, Dr. Fowler is an associate professor and director of research in the Division of General Internal Medicine and Geriatrics at IU School of Medicine and an implementation scientist at the Center for Health Innovation and Implementation Science.
About Regenstrief Institute
Founded in 1969 in Indianapolis, the Regenstrief Institute is a local, national and global leader dedicated to a world where better information empowers people to end disease and realize true health. A key research partner to Indiana University, Regenstrief and its research scientists are responsible for a growing number of major healthcare innovations and studies. Examples range from the development of global health information technology standards that enable the use and interoperability of electronic health records to improving patient-physician communications, to creating models of care that inform practice and improve the lives of patients around the globe.
Sam Regenstrief, a nationally successful entrepreneur from Connersville, Indiana, founded the institute with the goal of making healthcare more efficient and accessible for everyone. His vision continues to guide the institute’s research mission.
About IU School of Medicine
IU School of Medicine is the largest medical school in the U.S. and is annually ranked among the top medical schools in the nation by U.S. News & World Report. The school offers high-quality medical education, access to leading medical research and rich campus life in nine Indiana cities, including rural and urban locations consistently recognized for livability.