INDIANAPOLIS – An Expert Insight, published in the journal Transplantation, highlights health equity, disparity and inequality in organ transplantation along the continuum of care and across organ types. The authors provide a guide to transplant centers for the use of disparity-sensitive measures to monitor and address health disparities in transplantation and to redress long-standing inequities and inequalities in this vital arena.
 “Our goal is to ensure that all patients who need a transplant have an equitable opportunity to receive one, and if they do, to have an equitable opportunity to benefit from that transplant,” said the Expert Insight lead author Katie Ross-Driscoll, PhD, MPH, of the Regenstrief Institute and the Indiana University School of Medicine.
“Our goal is to ensure that all patients who need a transplant have an equitable opportunity to receive one, and if they do, to have an equitable opportunity to benefit from that transplant,” said the Expert Insight lead author Katie Ross-Driscoll, PhD, MPH, of the Regenstrief Institute and the Indiana University School of Medicine.
“While the U.S. healthcare system has mechanisms in place and we do a great job of measuring the quality of care provided to patients after organ transplantation, little is known about whether quality varies by patient characteristics even though we know that patient outcomes vary by these characteristics — by criteria such as race and ethnicity, and where patients live. When measuring transplant quality in current clinical practice or quality reviews, we want to make sure we are also measuring equity.”
Organ transplant centers in the U.S. already routinely collect information on the race, ethnicity and gender of transplant candidates and outcomes data on waitlisting and post-transplant survival. However, one notable gap in patient-level data collection, according to Dr. Ross-Driscoll, a health services researcher and epidemiologist, is the lack of inclusion of measures of socioeconomic status or social drivers of health.
This paper supplies transplant centers interested in using disparity-sensitive measures to monitor and address health disparities in transplantation with definitions of equity, disparity and inequality, which the authors note are often used interchangeably but are conceptually distinct. The paper also provides detailed guidance on how to measure equity within their processes across the spectrum of transplant care — from how they process referrals to how they measure their post-transplant outcomes.

“Patients, advocacy groups, researchers and others have called for transparency in the transplant process and a need for improving equity in the process patients must go through to get a transplant, how organs are procured and transplanted, and in outcomes,” said senior author Rachel Patzer, PhD, MPH, president and chief executive officer of Regenstrief Institute and Leonard Betley Professor of Surgery at the IU School of Medicine. “Recent national policy changes in transplant have emphasized improving transparency of reporting on referrals to transplant, time to transplant evaluation, and the time to organ procurement. The implementation of appropriate equity metrics is critical to have an impact on the population.”
All authors of “Health Disparity Metrics for Transplant Centers: Theoretical and Practical Considerations” and their affiliations:
Katie Ross-Driscoll1,2, Andrew Adams3, Juan Caicedo4, Elisa J Gordon5, Alan D Kirk6, Lisa M McElroy7, David Taber8, Rachel Patzer9 10.
1 Division of Transplantation, Department of Surgery, Indiana University School of Medicine, Indianapolis, IN.
2 Center for Health Services Research, Regenstrief Institute, Indianapolis, IN.
3 Division of Transplantation, Department of Surgery, University of Minnesota School of Medicine, Minneapolis, MN.
4 Division of Transplantation, Department of Surgery, Northwestern University School of Medicine, Chicago, IL.
5 Division of Transplantation, Department of Surgery, Vanderbilt University School of Medicine, Nashville, TN.
6 Department of Surgery, Duke University School of Medicine, Durham, NC.
7 Division of Transplantation, Department of Surgery, Duke University School of Medicine, Durham, NC.
8 Division of Transplantation, Department of Surgery, Medical University of South Carolina, Charleston, SC.
9 Regenstrief Institute, Indianapolis, IN.
10 Division of Transplant Surgery, Department of Surgery, Indiana University School of Medicine, Indianapolis, IN.
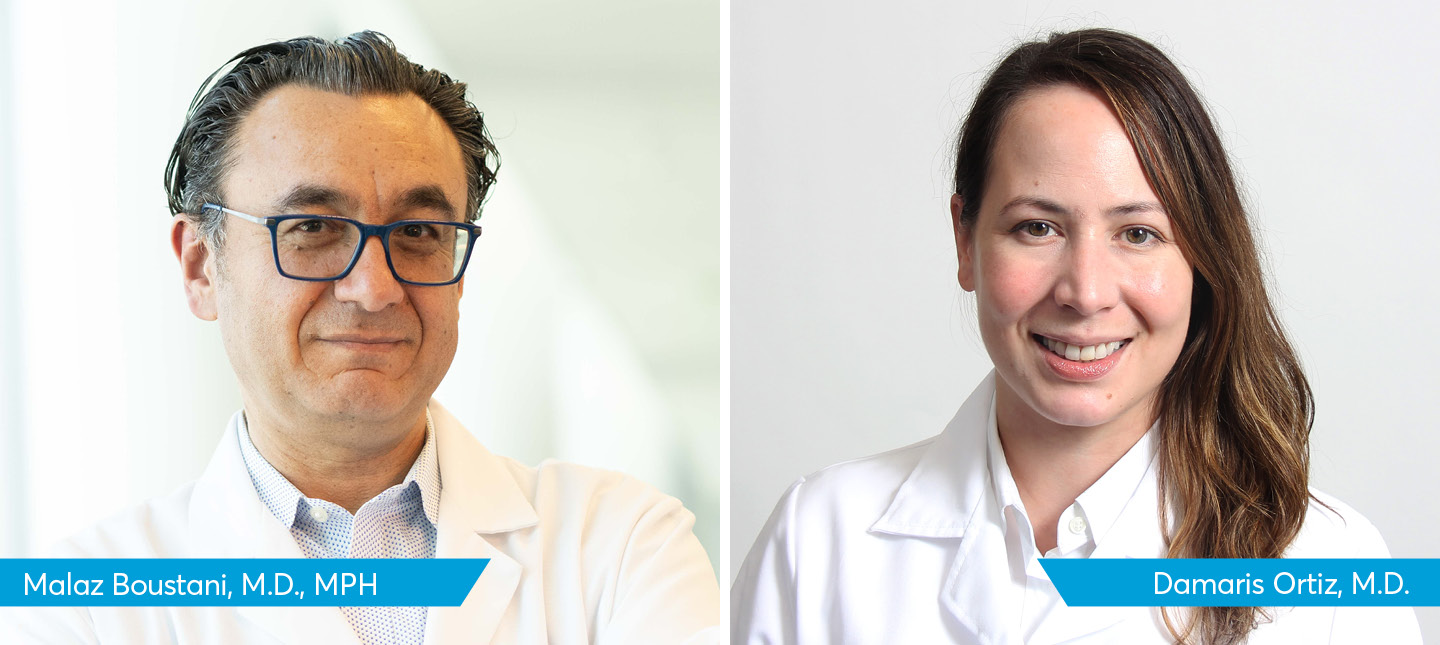
Katie Ross-Driscoll, PhD, MPH
In addition to her role as a research scientist with Regenstrief Institute, Katie Ross-Driscoll is an assistant professor of surgery at Indiana University School of Medicine. She is a health services researcher and epidemiologist focused on organ transplantation.
Rachel Patzer, PhD, MPH
In addition to her roles as president and CEO and research scientist with Regenstrief Institute, Rachel Patzer, PhD, MPH, serves as the Leonard Betley Professor of Surgery at Indiana University School of Medicine and an adjunct professor at IU Richard M. Fairbanks School of Public Health. Dr. Patzer is an epidemiologist and health services researcher with a strong focus on healthcare access, quality of healthcare delivery and outcomes. Her research centers on such key areas as disparities, social determinants of health, community-based participatory research, predictive analytics, healthcare quality and health policy evaluations. She has been instrumental in reshaping the national organ transplantation paradigm, advocating for a population health approach to inform quality measures, policies and equitable solutions.