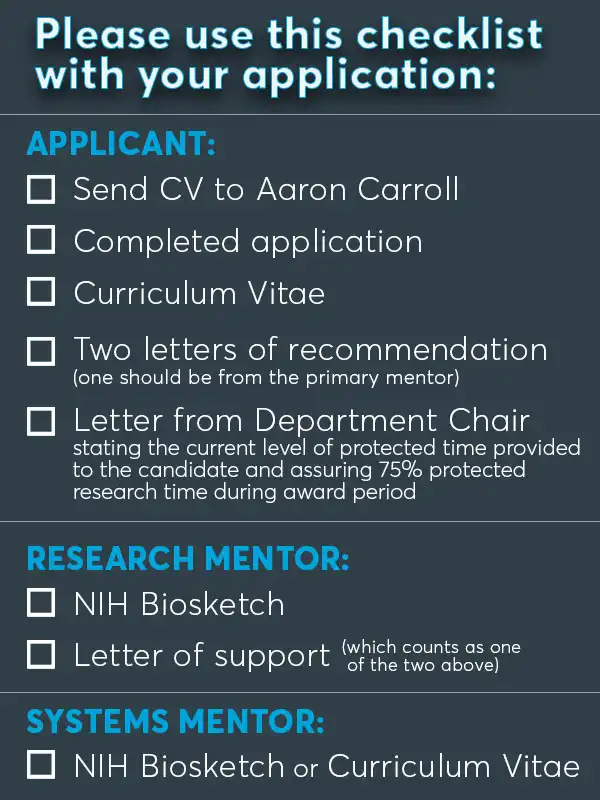
Candidates must e-mail a CV to Aaron Carroll for eligibility determination prior to submission of a full application online.
aaecarro@iu.eduClinical Investigator and Translational Education Program
Indiana University School of Medicine, IU Health, and the Regenstrief Institute are seeking applicants for The Learning Health System (LHS) Young Investigator Awards. These awards aim to train faculty to improve patient care and health system operations through the systematic generation, adoption and application of evidence. Clinicians and health system leaders work together to ensure that evidence is updated, disseminated to clinical teams and communicated to patients in ways that support shared decision making. Learning health systems are essential as the health care landscape becomes increasingly characterized by rich sources of information that are available in digital formats, programs, and applications.
As a new LHS Center of Excellence funded under an initiative from AHRQ/PCORI, this program will produce the next generation of LHS researchers to conduct patient-centered outcomes research and implement the results to improve quality of care and patient outcomes. Newly trained clinician and research scientists will work within health systems by collaborating with systems’ leaders and conducting studies to address how healthcare organizations can improve patient outcomes.
How to Apply
Before submitting an application:
- Forward a copy of your curriculum vitae to Aaron Carroll at aaecarro@iu.edu.
- We will review your CV to verify your eligibility to apply for this award.
Please be advised to complete this step as soon as possible.
Criteria for a successful application:
- Candidate must have two primary mentors, one from the research domain and one from the health delivery system domain.
- Candidate must have interest in using the learning health system to improve patient centered outcomes.
- Training plan (e.g., proposed courses, workshops, seminars, or other formal educational experiences relevant to the proposed research). Formal coursework may be important for applicants with a clinical doctoral degree, but less formal research training, than for individuals with a PhD or masters-level research degree.
- The research primary mentor must have a research program that is peer reviewed and extramurally funded.
- Department Chair must provide a letter assuring that the candidate will have 75% protected time during the award period.

Background & Instructions
The Learning Health System (LHS) Young Investigator Awards are designed to provide promising junior investigators the opportunity to be mentored to improve patient care and health system operations through the systematic generation, adoption and application of evidence. Clinicians and health system leaders work together to ensure that evidence is updated, disseminated to clinical teams and communicated to patients in ways that support shared decision making. Learning health systems are essential as the health care landscape becomes increasingly characterized by rich sources of information that are available in digital formats, programs, and applications.
Opportunities available to LHS Young Investigator Awardees
- Up to 75% salary support (capped at $75,000).
- $25,000 research funding per year of award for research, training and travel related
- Participation in Project Development Team practicum to enhance protocol development skills.
- Young Investigator workshops and coursework focused on research career development.
- Award is for 2 years (with 2nd year of funding contingent upon satisfactory progress during year one).
Program Plan
The LHS-K12 Training Program will be developed and implemented under the leadership of the Program Directors (Carroll/Embi), the LHS-K12 Executive Committee, and the Advisory Board (See Figure 1). The Program Directors and the Executive Committee will partner with our identified LHS primary mentors as well as the LHS Expert Panel, two of the cornerstones of our Career Development Plan for LHS-K12 Scholars. Each LHS-K12 scholar will be assigned two primary mentors, one from the research domain and one from the health system, who will oversee the scholar’s training curriculum and work closely with them on their experiential LHS Research Project, a required component of the LHS-K12 program. The LHS Expert Panel will supplement the guidance provided by the primary mentors, provide strong networking relationships for the scholar, and increase the depth of expertise, diversity, and views to which a scholar has access.
Eligibility
Individuals must meet ALL five (5) of the following criteria in order to apply:
- Applicants must fall into 1 of the following 2 categories:
- Clinician-scientist with a doctoral degree (physicians, nurses, dentists, pharmacists, clinical psychologists, optometrists, veterinarians, allied health care professionals, etc.).
- Basic or other non-clinician scientist with a PhD who is doing LHS research and has high potential for early translation into impacting patient care.
- Only U.S. citizens and permanent residents are eligible to apply.
- Applicants must be an Assistant Professor at the time of the award (1 July 2021), and within the first 5 years of his or her faculty appointment. Appointments cannot be contingent upon receipt of the K12 award.
- Applicants must be able to commit a minimum of 75 percent of full-time professional effort to conducting research and to any training activities associated with the program. The remaining 25 percent effort can be divided among other research, clinical and teaching activities only if these activities are consistent with the proposed goals of the K12 program. However, this 25 percent effort may not be supported by other federal grants.
- Applicants may not simultaneously submit or have pending an application for any other PHS mentored career development award (e.g., K01, K07, K08, K22, K23) or career development award equivalent. Former or current principal investigators on an R01 or other major NIH research grant are NOT eligible to apply. Note that this does not include NIH Small Grants (R03) or Exploratory/Developmental (R21) grants or their equivalents. Also, individuals who have been a PI on grants from any source for which an eligibility criterion is “independent status” and/or the annual direct costs are ≥ $250,000 are NOT eligible.
Executive Committee
The executive committee will serve a number of operational and coordinating functions and roles by assisting the program directors in: a) identification, evaluation and recruitment of Scholars, b) overseeing the mentorship of Scholars, and c) enabling the conduct of research within the learning health system. The Executive Committee will be responsible for identification of new initiatives related to LHS research at IUSM/IU Health, establishment of relevant policies and procedures, and training program development and revision. Finally, members of the Executive Committee will also serve as “content experts” for one or more of the AHRQ core competency domains (See Section B.4.c). They will each be responsible for updating educational offerings in that domain, making sure that the curriculum offered to Scholars covers those domains adequately, and for making sure that personal educational plans are adequate to those domains. The committee will be chaired by co-Program Director, Peter Embi, and will meet monthly.
Program Directors
 Aaron Carroll, MD
Aaron Carroll, MD
Aaron Carroll, MD, MS
Dr. Carroll is the Director of the Center for Pediatric and Adolescent Comparative Effectiveness Research (PACER) and Professor of Pediatrics at IUSM. He has published extensively and received funding through R01-level grants from AHRQ, NIDDK and NLM. He has mentored more than 30 mentees and serves as the Associate Dean for Research Mentoring, reporting directly to the School of Medicine’s Executive Dean of Research with a mandate to assist junior faculty in developing their research careers. Dr. Carroll brings to this proposal expertise in patient recruitment, patient-centered research methods including qualitative research approaches, health information technology, clinical decision support, health policy, and health communication messaging including communicating with health care consumers through a variety of media outlets (print media, YouTube, blogs, etc.). He has been awarded a Patient-Centered Outcome Research and Comparative Effectiveness Research Infrastructure Development Grant (R24) from AHRQ that created the infrastructure to support cores which will be integral to the human-centered design portions of this proposal.
 Dr. Titus Schleyer
Dr. Titus Schleyer
Titus Schleyer, DMD, PhD
Dr. Titus Schleyer is a Research Scientist in Regenstrief’s Center for Biomedical Informatics and Professor of Biomedical Informatics at IU School of Medicine. He leads the Indiana Learning Health Systems Initiative, which is focused on using everyday patient care data to improve the health of and healthcare for people in Indiana. Dr. Schleyer is working to make information from various sources more accessible and useful to clinicians. One of his award-winning projects provides ED physicians with highly relevant information about their patients from Indiana’s major health information exchange directly in the electronic health record. Dr. Schleyer is also active in big data analytics for population health management. In addition to recently receiving a Regenstrief Institute Outstanding Investigator Award, Dr. Schleyer was recognized for his teaching and mentorship with a Indiana University Trustee Teaching Award in 2020. He co-directs the National Library of Medicine-funded Public & Population Health Informatics (PHI) Fellowship at Indiana University.
 Dr. Malaz Boustani
Dr. Malaz Boustani
Malaz Boustani, MD, MPH
Dr. Boustani is a senior implementation scientist with extensive experience in mentoring junior investigators and conducting implementation research with a main focus on developing tools, processes, and strategies to rapidly implement evidence based and cost effective health care solutions in the real world. He has used this clinical laboratory to train more than 15 clinical investigators who have successfully received Career Development Awards and 4 of them have already became independent principal investigators of R01 equivalent awards from the NIH. Furthermore, Dr. Boustani has coached more than 50 emerging healthcare leaders in innovation, implementation science, change management, and system thinking. These leaders have been embedded within multiple healthcare systems as change agents and catalysts for healthcare transformations. Dr. Boustani will serve as the “content expert” for the Improvement and Implementation Science core competency domain of the LHS-K12 program.
 Christopher Weaver, MD, MBA
Christopher Weaver, MD, MBA
Christopher Weaver, MD, MBA
Dr. Weaver is Associate Professor of Emergency Medicine at Indiana University School of Medicine and Senior Vice President (SVP) of Clinical Effectiveness at Indiana University Health. He has extensive experience in leading complex and large initiatives within various healthcare delivery systems. For a decade he was the chief Medical Officer (CMO) and the Chief Operation Officer (COO) at Eskenazi Health, a safety net urban integrated healthcare delivery organization. At Eskenazi, Dr. Weaver transformed Eskenazi Hospital into a learning organization capable of implementing scalable and sustainable evidence-based services such the collaborative care models for frailty, dementia, and depression. Dr. Weaver used his competencies in business operation and care delivery logistics to successfully implement two system wide major care transformations; transitional care and population health management models across the entire clinical integration network supported by Marion County including several hospitals, community health centers, mental health centers, nursing homes, emergency medical services, and department of health. In 2017, Dr. Weaver accepted a new enterprise position at Indiana University Health as the SVP of Clinical Effectiveness. The scope of his new role is to leverage the academic expertise and knowledge of the faculty of IUSM to transform IU Health into a learning healthcare system serving the entire state of Indiana. Dr. Weaver has the training, leadership experience and organizational role to be a member of the Executive Committee and to serve as the “content expert” for the System Science core competency domain in this proposal. In addition to guiding health systems through constant changes, he has successfully mentored many individuals in a variety of roles including medical students, residents in training, health administration graduate students, school of medicine faculty, and leaders of health systems.
 Shaun Grannis, MD, MS VP for Data and Analytics
Shaun Grannis, MD, MS VP for Data and Analytics
Shaun Grannis, MD, MS, FAAFP
Dr. Grannis is Vice President for Data and Analytics and a Research Scientist at Regenstrief Institute. He has been a close collaborator with national and international public health stakeholders to advance the technical infrastructure and data-sharing capabilities. He served as a member of World Health Organization (WHO) Collaborating Center for the Design, Application, and Research of Medical Information Systems, where he provided consultancy on issues related to health information system identity management; and implementing automated patient record matching strategies. He has built and studied automated regional electronic laboratory reporting systems that demonstrate substantial increases in the electronic capture rates for diseases of public health significance when compared to traditional, manual, paper- based procedures, despite substantial data quality challenges. He also oversees the evaluation of operational standards-based laboratory data interfaces between public health clinical laboratories and an electronic clinical messaging application used by both public health officials and clinicians. As co-chair of the U.S. Health Information Technology Standards Panel (HITSP) Population Health technical work group, he has helped lead development of technical Interoperability Specifications for nationally recognized public health IT use cases. Dr. Grannis also served as the Director of the Indiana Center of Excellence in Public Health Informatics, one of only four such centers of excellence in the United States. Dr. Grannis has received AHRQ R01 funding to develop methodological improvements for real-world patient matching systems. His recent research focuses on developing and testing large-scale HIE- based solutions in support of population health and public health informatics; integrating clinical and social determinants of health (SDH) to identify at-risk patients in need of SDH services, which include nutrition counseling, financial planning, and medical-legal partnership assistance; developing and testing novel patient matching methods; and leveraging machine learning-based models to improve discovery and decision support in a variety of contexts. He also serves as Chief Architect for OpenHIE, a global health collaborative supporting eHealth planning and implementation needs for developing countries. Dr. Grannis will serve as the “content expert” for the Informatics core competency domain.
 Peter Schwartz, MD, PhD
Peter Schwartz, MD, PhD
Peter Schwartz, MD, PhD
Dr. Schwartz is the Director of the Indiana University Center for Bioethics and associate professor of medicine at IU School of Medicine, and practices adult internal medicine at Eskenazi Health. He writes about ethical issues and conducts empirical research on risk communication and shared decision-making in prevention and precision medicine. He is currently PI of a project on comparative effectiveness of methods of risk communication regarding colorectal cancer screening, funded the Patient Centered Outcomes Research Institute (PCORI). As Director of the Bioethics and Subject Advocacy Program of the Indiana Clinical and Translational Sciences Institute (CTSI) he instructs and mentors students, trainees, and junior faculty in responsible conduct of research, ethics, and research in patient decision making. As associate professor of philosophy at Indiana University Indianapolis, he teaches regularly in the MA program in bioethics. Dr. Schwartz will serve as the “content” expert for the Ethics of Research and Implementation in Health Systems core competency domain.
 Sarah Wiehe, MD, MPH
Sarah Wiehe, MD, MPH
Sarah Wiehe, MD, MPH
Dr. Wiehe is the Director of Community Health Partnerships (CHeP) and the Patient Engagement Core at the Indiana CTSI and Associate Professor of Pediatrics at IUSM. She has published extensively and received funding through R01-level grants from NIH, AHRQ, and PCORI. She has mentored 20 pre- and post-doctoral trainees and 17 junior faculty. Of the 11-junior faculty she mentors currently, 2 have institutional K awards, 1 has an NIH K award, and 6 have NIH K awards under review. Dr. Wiehe brings to this proposal expertise in community and stakeholder engagement, user-centered design research, epidemiology and health services research, and creative use and linkage existing data to address both individual and population health issues. She will serve as the “content expert” for the Engagement, Leadership, and Research Management core competency domain.




