INDIANAPOLIS – A commentary published in the Journal of Neurotrauma calls for traumatic brain injury to be recognized as a chronic condition as are diabetes, asthma, depression and heart failure.
INDIANAPOLIS – A commentary published in the Journal of Neurotrauma calls for traumatic brain injury to be recognized as a chronic condition as are diabetes, asthma, depression and heart failure.
To provide comprehensive care for traumatic brain injury throughout individuals’ lifespans, the authors propose that coordinated care models they and others have developed, tested and applied to various populations — including older adults, individuals living with depression and post-intensive care unit survivors — be adapted to improve communication and integration between brain injury specialists — including physical medicine and rehabilitation clinicians — and primary care physicians, fostering better long-term patient care for traumatic brain injury survivors and more support for both patients and their families.
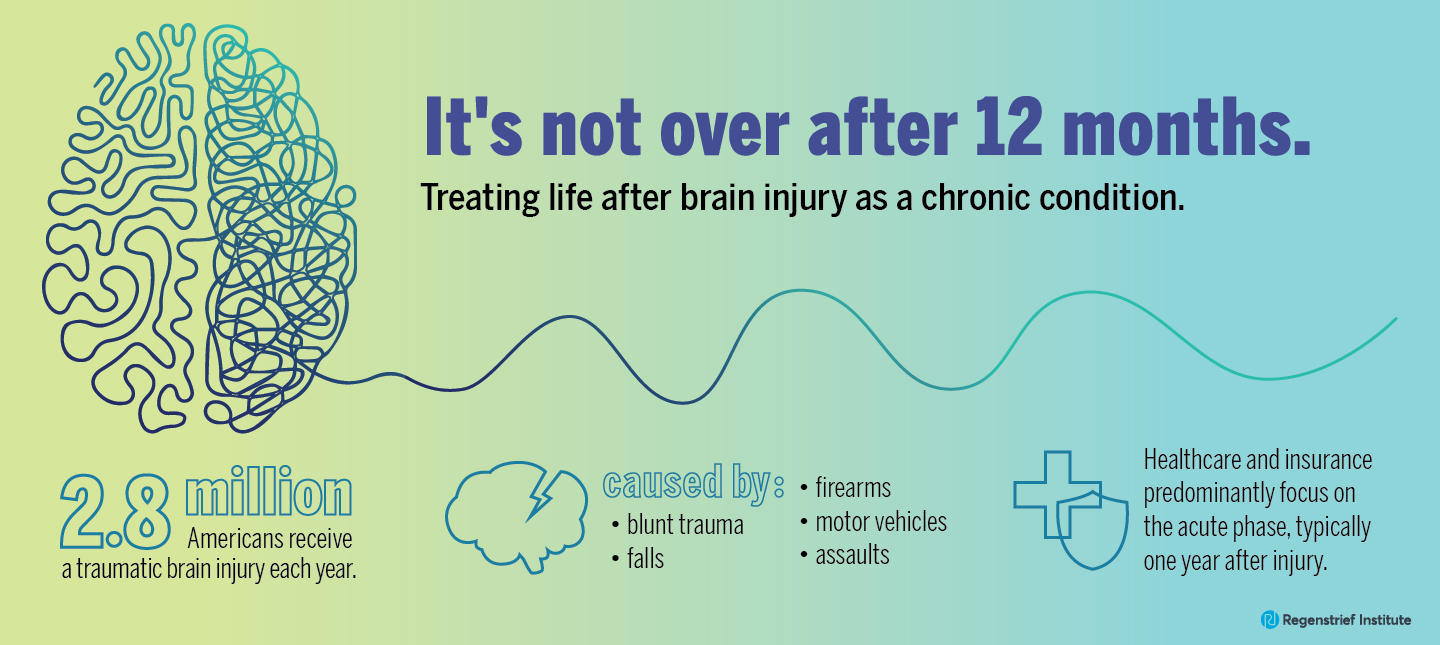
The incidence of traumatic brain injury (frequently referred to as TBI) is rising in the U.S., with an estimated 2.8 million Americans receiving a traumatic brain injury each year. The healthcare system and insurance coverage predominantly focus on the acute phase of the condition, typically the first year after the injury is sustained. But for a significant number of those living with a traumatic brain injury, the effects are long lasting, occurring for a lifetime. Post-acute care options, however, are often rather bleak.
Traumatic brain injury is most commonly caused by falls (especially in older adults), blunt trauma (particularly sports-related injuries), firearms, motor vehicles or assaults. Damage can be confined to one area of the brain or it can occur over a more widespread area. Many factors including the size, severity and location of the brain injury as well as age of the individual and prior brain injuries impact recovery.
According to the Centers for Disease Control and Prevention, populations more likely to be affected by traumatic brain injury include:
- racial and ethnic minorities
- service members and veterans
- people who experience homelessness
- people who are in correctional and detention facilities
- survivors of intimate partner violence
- people living in rural areas
The commentary authors observe that many clinicians believe that residual impairments due to traumatic brain injury are static once initial recovery has plateaued and do not expect significant changes over the remainder of a person’s life. In contrast, the commentary authors write that the long-term course of traumatic brain injury involves waxing and waning and thus could be better characterized as dynamic rather than static. Accordingly, they call for traumatic brain injury to be considered and managed as a chronic condition.
“Acknowledging traumatic brain injury as a chronic condition and providing coordinated care will make a difference to patients, their families and to how the healthcare system operates in several ways. It recognizes that for many patients it’s not over after 12 months and, importantly, provides these patients with a place of care where they can be monitored and helped over many years,” said commentary senior author Kurt Kroenke, M.D. of the Regenstrief Institute and the Indiana University School of Medicine.
“Recognizing TBI as a chronic condition and using coordinated care models support the important role of self-management for both the patient and their family. These two steps facilitate collaboration between the limited number of brain care specialists and the primary care clinicians who typically oversee care throughout the TBI survivor’s lifetime. Collaborative care models, which we at Regenstrief Institute and others have developed, provide patients living with chronic conditions with the support and coordinated care they need. Medicare recently recognized TBI as one of 18 chronic conditions, hopefully others will follow.”
Dr. Kroenke notes that the chronic condition designation by Medicare opens the door to change in how traumatic brain injury is managed long-term and may guide healthcare systems to better integrate brain injury specialists — who are in short supply — with primary care providers through collaborative care models. It may also encourage health insurers to provide coverage for the many years of care needed by some survivors.
“We can improve life after brain injury with a more proactive approach and a longer-term view of brain injury as a chronic and dynamic condition. This approach anticipates changes over time and incorporates strategies to optimize healthy living with coordinated care that is individualized for the lifetime needs of those living with brain injury,” said commentary co-author Flora M. Hammond, M.D., Covalt Professor of Physical Medicine and Rehabilitation and Chair of the Department of Physical Medicine and Rehabilitation at the IU School of Medicine.
“Recognition of TBI as a chronic condition would not only focus more resources on problems associated with living with brain injury but would also enhance both the public’s and professionals’ awareness of how to optimize the health and well-being of persons living with the effects of TBI,” the commentary concludes.
“Recognition of Traumatic Brain Injury as a Chronic Condition: A Commentary” is published in the Journal of Neurotrauma.
Article authors and affiliations
John D. Corrigan, PhD1, Flora M. Hammond, M.D. 2, Angelle M. Sander3, and Kurt Kroenke, M.D.4.
1Department of Physical Medicine & Rehabilitation, The Ohio State University, Columbus, Ohio, USA.
2Department of Physical Medicine and Rehabilitation, Indiana University School of Medicine, Indianapolis, Indiana, USA.
3H. Ben Taub Department of Physical Medicine and Rehabilitation, Baylor College of Medicine, and Brain Injury Research Center, TIRR Memorial Hermann, Houston, Texas, USA.
4Department of Medicine, Indiana School of Medicine and Regenstrief Institute, Indianapolis, Indiana, USA.
Kurt Kroenke, M.D., MACP
In addition to his role as a research scientist with the William M. Tierney Center for Health Services Research at Regenstrief Institute, Dr. Kroenke is also an Indiana University Indianapolis Chancellor’s professor and a professor of medicine at the Indiana University School of Medicine.